Background
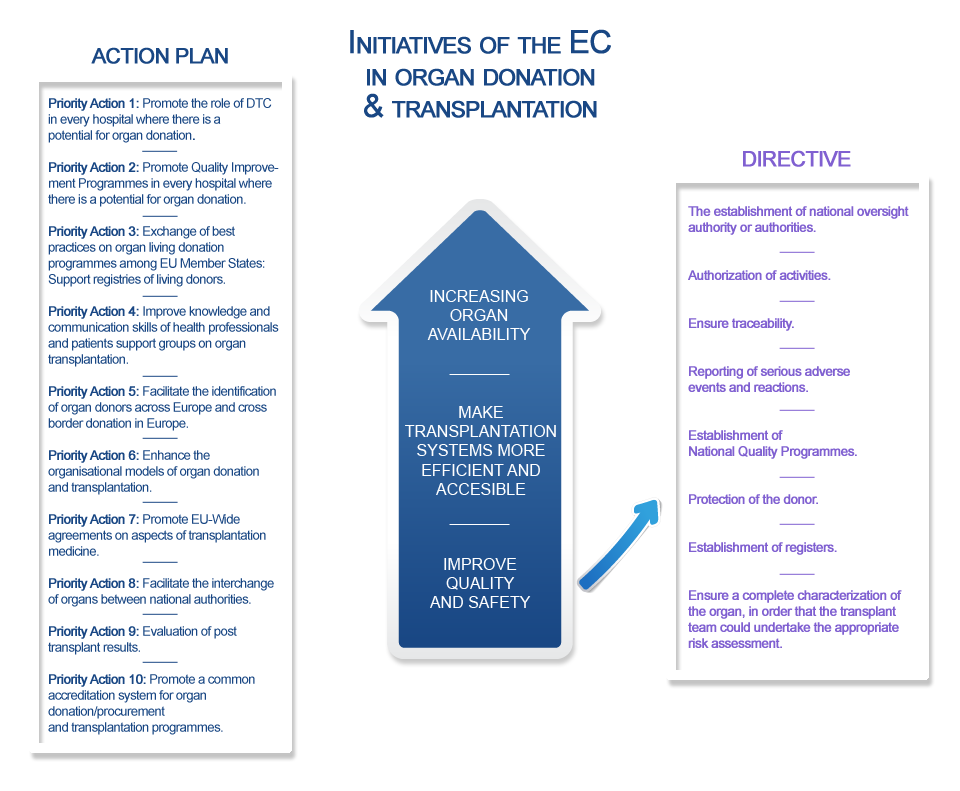
Organ transplantation (OT) benefits about 28,000 patients in the European Union (EU) yearly, but the availability of organs does not meet the OT needs, unequally met by Member States, mainly due to variability in living and deceased donation rates. This heterogeneous scenario and the need to establish a common framework for quality and safety of human organs intended for OT, has led to two EU initiatives in the field: Directive 2010/53/EU (the Directive) and the Action Plan on Organ Donation and Transplantation (2009-2015): Strengthened Cooperation between Member States, with ten identified priority actions. Live donation activity is increasing in the EU to better meet the OT needs. But the live donor faces risks which make mandatory an appropriate framework of donor care in compliance with universal standards. These include the development of a live donor registry, as set down in the Directive, essential to build evidence on the consequences of donating an organ during lifetime, but not yet available in many Member States. The main reason justifying differences in deceased donation rates across countries is failure to identify potential organ donors. A close cooperation between intensive care professionals, dealing with end-of-life care, and donor transplant coordinators, is fundamental to possible donors becoming actual donors, as put forward in the WHO critical pathway. Nevertheless, the integration of donation in end-of-life care remains a challenge. Providing recommendations on how to build this integration, based on a benchmarking approach, has proven effective in different countries, but must be respectful with differences in end-of-life patterns of care. Finally, international cooperation is considered per se an effective tool to improve performance in donation and OT practices. Twinning activities may promote that the experience and knowledge developed by one Member State is transferred to others who request such transference and will implement the advance willingly. In this framework, ACCORD will address these challenges by working in 3 specific areas:
- The development of live donor registries
- The cooperation between intensive care and donor transplant coordinators
- Twinnings in the fields specified by the Directive and the Action Plan